An episode of the Dr. Oz Show, which aired on October 3rd, 2013, featured an investigative report about the potential life-long side effects of LASIK eye surgery.
As a popular elective surgery, nearly 800,000 people get Lasik every year. FDA clinical data trial shows that every modern laser left 1 out of 5 patients seeing worse after LASIK. Side effects include seeing double, seeing halos or starbursts (especially at night), and dry eye pain.
Investigative reporter Elisabeth Leamy has been investigating the harmful side effects of LASIK for over two years. During her undercover consultations with doctors, she discovered that the side effects were minimalized and the procedure was treated like an easy, no-risk procedure.
Morris Waxler, the former FDA official responsible for getting LASIK surgery approved, is now working to get it banned. He says that the side effects of LASIK are actually injuries and that LASIK harms 20% of patients.
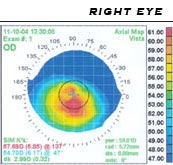
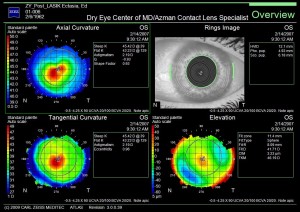
LASIK eye surgery works by cutting a flap of the top layer of the cornea and then using a laser to reshape the exposed cornea. Complications can occur when the flap of the cornea is cut too thick, too thin or too far into the cornea. However, even if this cut is perfect, when the flap is put back down it doesn’t necessarily heal perfectly. Years later it can become dislodged and trigger negative side effects. In addition, if there were underlying issues prior to the LASIK surgery that were not treated, LASIK surgery (and enhancement touch-ups) will most likely exacerbate the issues. Unfortunately many post LASIK patients now have life long side effects, ranging from the smallest amount to the most severe.
Dr. Irwin Azman provides treatment for people who underwent LASIK, PRK, and RK sugery but are now experiencing post-surgical side effects and complications.
According to Dr. Azman:
“While LASIK surgery can be successful under optimum eye conditions, unfortunately many patients do experience side effects due to pre-existing conditions. However, there is hope. Utilizing our vast experience and expertise, as well as an array of new technologies, we are able to treat these side effects with non-surgical techniques.”