LASIK (Photo credit: Wikipedia)
When people hear the term “laser eye surgery”, the first thing they think of is LASIK. However, most people are not aware that LASIK is not the only “laser eye surgery”. The other laser eye surgery options include PRK, LASEK, and IntraLase. Each of these optionshas an excellent safety record, and high success rates. These surgeries are intended to treat myopia (nearsightedness), hyperopia (farsightedness) and astigmatism, and, unbelievably, can allow you to lead a life without glasses or contact lenses. Although severe LASIK complications and LASIK failures such as complete or partial loss of vision are extremely rare, many side effects can occur.
Like all other surgical procedures, there are potential risks and side effects. LASIK complications commonly include, glare, halo’s and other issues, which are delineated below. LASIK failures and LASIK complications can occasionally be resolved with additional surgery; however more surgery can exacerbate the symptoms.
LASIK Eye Surgery Risk Factors and Limitations
Not every patient is a candidate for LASIK. Specific health and eye conditions and anatomical factors can put you at an increased risk for LASIK complications and LASIK failures. These conditions include, thin or irregular corneas, large pupil size, your specific degree of refractive error, whether or not you suffer from dry eyes; your age, whether your vision is stable, whether you are pregnant, and if you have specific degenerative or autoimmune disorders.
Post LASIK Side Effects and Complications
Although LASIK eye surgery has been performed on millions of people in the United States, experienced LASIK surgeons report that serious complication rates can be held below one percent. However, like any surgical procedures, there are potential risks and side effects. LASIK failures and LASIK complications commonly include, glare, halos, dryness, ghost images, star bursting, smeared images, loss of contrast, vision fluctuation, blurry vision, and double vision. LASIK failures and LASIK complications can occasionally be resolved with additional surgery, but often exacerbate the problem.
Vision disturbances: Halos, glare and starbursts in low vision, especially at night; dry eye symptoms; hazy vision; and reduced sharpness of vision.
Flap complications: One of the crucial steps in LASIK surgery is the creation of a thin hinged flap on the front surface of the cornea. In the course of the surgery the flap is lifted for the laser to reshape the cornea. The flap is then replaced and heals naturally. If the flap is not made correctly, it may fail to keep to the eye’s surface causing corneal striae. These LASIK flap complications can lead to an irregularly shaped cornea and cause distorted vision.
Other problems associated with LASIK flap complications include:
- Irregular astigmatism: Caused by an unequally curved corneal surface. Resulting symptoms may include double vision or “ghost images.”
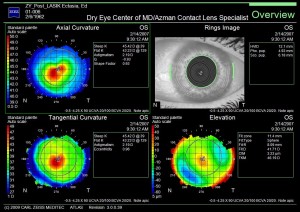
- Keratectasia or Keratoconus: Bulging of the cornea can occur when too much tissue is removed during the LASIK procedure. Or when the cornea, prior to LASIK is weak as evidenced from corneal topography mapping. Rarely does keratoconus develop after LASIK with no known risk factors. Enhancement laser surgery is usually not suitable, and scleral contact lenses, gas permeable contact lenses or, corneal implants may be prescribed.
Left: Post LASIK uncorrected HOAs with starbursts at night.
Right: Corrected Post LASIK HOAs at night
Dry eyes after LASIK: LASIK surgery can cause a decrease in tear production and cause your eyes to feel scratchy and blurry. Almost half of all patients experience some degree of temporary dry eye syndrome. People who already have severe dry eye should have been eliminated as LASIK candidates.
Significant under-correction, overcorrection or regression. Not all patients will patients will receive 20/20 vision after LASIK eye surgery, and contact lenses or glasses for some or all activities may still be required. If the laser removes too much or too little corneal tissue, or you do not have typical healing, your best vision outcome can be less than optimal. Furthermore, if the laser removes tissue in an uneven manner or your eye heals unevenly, astigmatism can result.
LASIK Failures and LASIK Complications: | |
Complications | Symptoms |
| Incomplete corrections (under-correction, over-correction, residual astigmatism) or regression of effect | Blurry, less-than-perfect vision |
| Decentered ablations | Visual distortions & aberrations (HOA) |
| Oversize pupils | Visual distortions & aberrations (HOA) |
| Haze | Visual distortions & aberrations (HOA) |
| Irregular flap | Visual distortions & aberrations (HOA) |
| Dry eye | Dry, itchy or scratchy eyes. |
| Diffuse lamellar keratitis (eye inflammation) | Visual distortions & aberrations (HOA) |
Dr. Irwin Azman has over 25 years of experience in the diagnosis and management of the Post LASIK patient with LASIK failures and LASIK complications. Dr. Azman utilizes non-surgical restoration techniques to restore quality vision to those who have lost it due to LASIK failures and LASIK complications, R-K surgery, corneal transplant surgery, ocular trauma, dry eye and corneal disease. Together with his knowledge and experience, his team of technicians, new technologies in instrumentation and new treatment modalities, Dr. Azman is able to prescribe each LASIK failure patient with the perfect solution in resolving their LASIK complications, without any further surgical procedures.